POSTED IN: General Info, Long-Term Care
TAGS: Health & Nutrition, Long-Term Care Facilities, Nursing Home
Share this
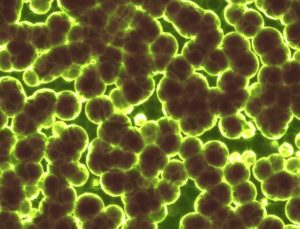
A superbug is defined as a pathogenic microorganism, especially a bacterium, that has developed resistance to the medications normally used against it. Hospitals and nursing homes are able to keep lethal superbug outbreaks a secret, due to vague rules that give healthcare providers great leeway in deciding when or whether to report unusual clusters of infections. The public is not generally informed of outbreaks, leaving patients, their families and the broader public ignorant of potentially deadly threats. A recent Reuters investigation found dangerous flaws in efforts to control the spread of superbug infections. Every year, thousands of Americans are sickened and thousands die from infections by antibiotic-resistant bacteria and C. difficile, a pathogen linked to long-term antibiotic use. The Centers for Disease Control and Prevention says: About two million people get sick every year with antibiotic-resistant infections in the United States and about 23,000 die. One in 25 U. S. hospital patients has caught an infection while in the hospital.
Timely reporting of outbreaks of these infections is essential to stopping the spread of disease and saving lives, public health experts and patient advocates say. The United States lacks a unified nationwide system for reporting and tracking outbreaks, leaving a patchwork of state laws and guidelines, inconsistently applied, to track clusters of the deadly infections that the federal government labeled “a grave threat to public health” 15 years ago. Therefore, there is no way to count the deadly spikes in infections that hit the nation. Reuters assembled a comprehensive count from 29 state health departments, identifying at least 300 superbug outbreaks around the nation from 2011 to 2016, affecting a number of people impossible to count.
A major problem exists in long-term care facilities. Isolation of an affected resident in a nursing home is most practical, however, very few nursing homes follow the recommended isolation precautions for residents with multi-drug resistant infections, placing other residents at risk of the serious and potentially life-threatening superbug infections. A study published last month in The Journal of the American Geriatrics Society, by Columbia University School of Nursing, found that isolation procedures were used on only about 13% of all nursing home infection cases involving drug-resistant strains. The study involved 200,000 nursing home residents with multidrug-resistant organism (MDRO) infections, in which researchers determined that Isolation was infrequently used. Isolation precautions include: placing nursing home residents in private rooms, or having them wear protective clothing. These steps are designed to prevent the spread of infections by superbugs which are especially dangerous to elderly residents of long-term care facilities as well as those with compromised immune systems.
The federal Centers for Medicare & Medicaid Services mandates that hospitals and long-term care facilities participating in the huge government insurance programs provide all necessary medical information when a patient is being transferred. However, the state outbreak reports that Reuters reviewed showed that hospitals and nursing homes often do not alert each other when they transfer an infected patient, which can allow contagion to spread among multiple locations. Reuters documented cases in which infected patients were transferred, sometimes multiple times, without any of the receiving facilities being notified. In some cases, the transferring facility knew of the infections. In others, it was unaware. State outbreak reports often lack basic information, such as how many people were affected, the source of the outbreak, or when it began or ended. In 16 states, the name of the facility must be removed from the report by law before it is released.
Long-term care facilities — nursing homes, rehab centers and the like — are particularly vulnerable to outbreaks. A Reuters analysis of death certificates found that from 2003 to 2014, annual superbug-related deaths at long-term care facilities increased 62 percent, from about 1,400 to almost 2,300. Patients in these facilities are ideal superbug targets — the chronically ill, the very old, and anyone else with a compromised immune system. Collected under one roof, these people are easy prey.
For more information go to:
http://www.reuters.com/investigates/special-report/usa-uncounted-outbreaks/
http://atlanticcity.legalexaminer.com/nursing-home-elder-abuse/nursing
…
Share this
Subscribe to our blog and monthly newsletter.